SmartPAN
Health and Cost Effectiveness Modelling Pancreas Type A-D
The Model1
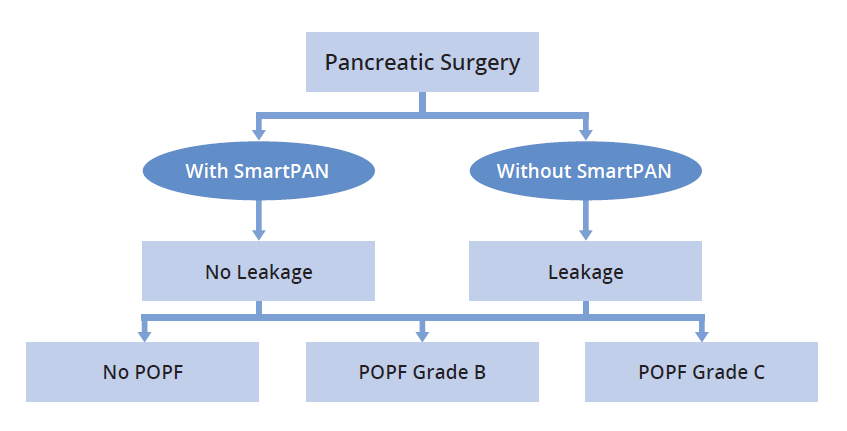
- The Health and Cost Effectiveness model was developed by the Swedish Institute for Health Economics
(IHE, www.ihe.se). IHE is a health economic research centre in Sweden with a large team of health
economists. IHE collaborate with national authorities, pharmaceutical companies, healthcare providers,
branch organisations, and patient interest groups. - The probability of leakage following pancreatic surgery is sourced from the study by Nahm et al.2 in which
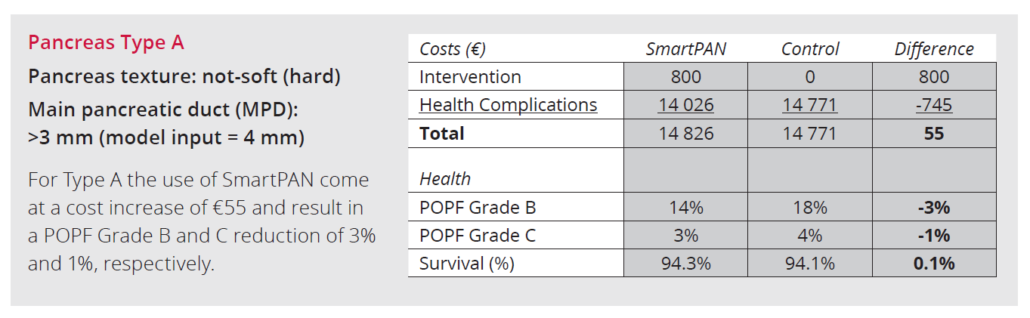
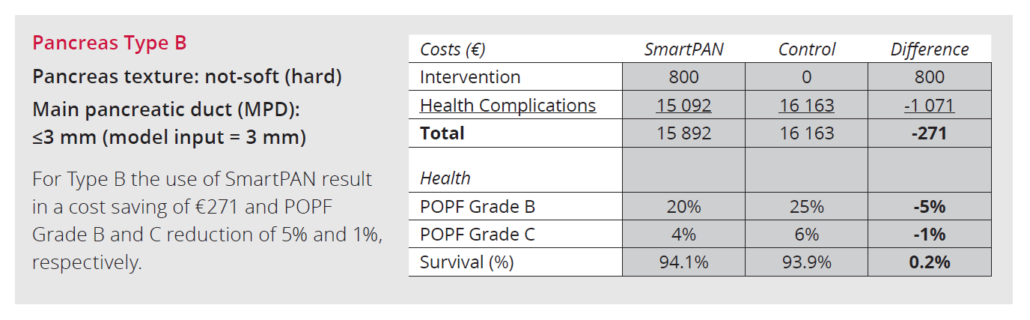
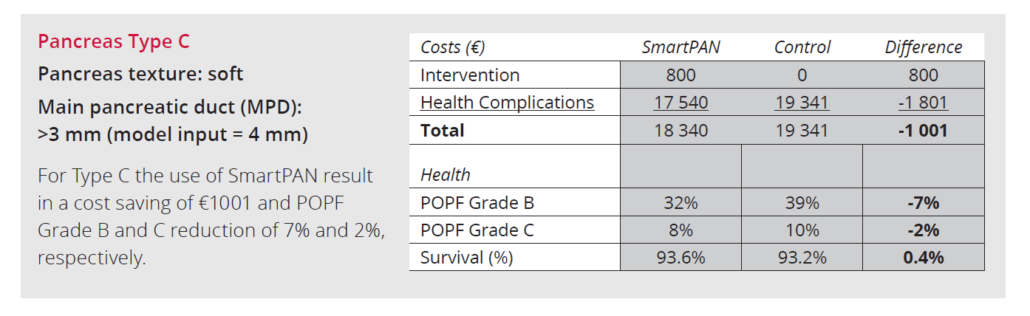
leakage was defined by intraoperative amylase concentration > 1000 U/L. - The underlying risk of developing POPF is based on the Alternative Fistula Risk Score for
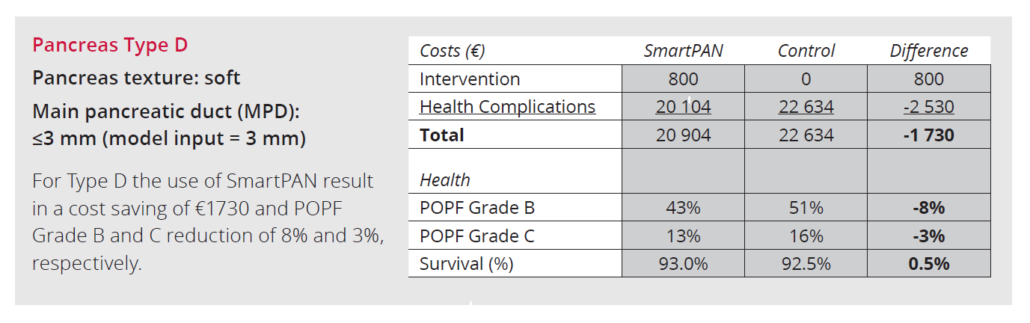
Pancreatoduodenectomy (a-FRS) 3. Classification of Pancreas type A-D according to the International
Study Group of Pancreatic Surgery (ISGPS) 4. Underlying BMI is set to 25 in the model. An additional
increase in BMI leads to increased POPF risk and cost effectiveness of SmartPAN. - The risk of clinically relevant POPF is split to Grade B and Grade C using the reported number of Grade B
and Grade C in the study by McMillan et al.5 - The impact of leakage for the risk of developing POPF is included in the model as an odds ratio. The
model default is an odds ratio of 2.0 sourced from a study by Wang et al.6 and consider the risk of
developing POPF Grade B and Grade C compared with no POPF. - Daily costs of No POPF, POPF Grade B, and POPF Grade C is sourced from the Italian study by Pulvirenti et al.7
The Model1
References
- SmartPAN Cost Effectiveness Model for Pancreatic Surgery. DOC-03489, data on file.
- Nahm C.B et al., Intra-Operative Amylase Concentration in Peri-Pancreatic Fluid Predicts Pancreatic Fistula After Distal Pancreatectomy.
J Gastrointest Surg, 2017. 21(6): p. 1031-1037. - Mungroop T.H et al., Alternative Fistula Risk Score for Pancreatoduodenectomy (a-FRS): Design and International External Validation.
Ann Surg, 2019. 269(5): p. 937-943. - Schuh F et al., A Simple Classification of Pancreatic Duct Size and Texture Predicts Postoperative Pancreatic Fistula: A classification of
the International Study Group of Pancreatic Surgery. Ann Surg. 2023 Mar 1;277(3):e597-e608. - McMillan M.T., et al., Risk-adjusted Outcomes of Clinically Relevant Pancreatic Fistula Following Pancreatoduodenectomy: A Model for
Performance Evaluation. Ann Surg, 2016. 264(2): p. 344-52. - Wang W et al., Has the pancreatic fistula already occurred in the operation? An intraoperative predictive factor of clinical relevantpostoperative
pancreatic fistula after the distal pancreatectomy. Surg Open Sci, 2019. 1(1): p. 38-42. - Pulvirenti A et al., Clinical Implications of the 2016 International Study Group on Pancreatic Surgery Definition and Grading of
Postoperative Pancreatic Fistula on 775 Consecutive Pancreatic Resections. Ann Surg, 2018. 268(6): p. 1069-1075.